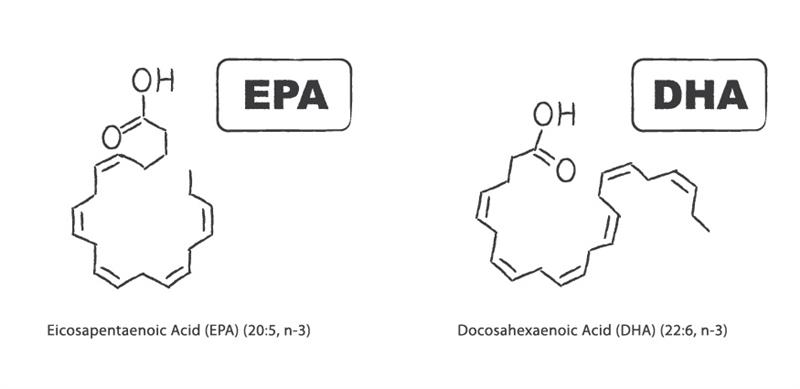
For the most part, EPA and DHA have been considered to have similar health benefits; therefore, the various dosing recommendations usually describe a combination of the two (EPA plus DHA), without differentiation. However, over the past decade a number of studies have shown both mechanistic and clinically-relevant differences between these two similar fatty acids, leading to potential targeted therapeutic uses for each. In some cases, there are head-to-head comparisons between the two in clinical trials; in other cases, there are epidemiological or basic science discoveries that are driving clinical focus on one fatty acid over the other for particular health concerns.
It is often thought that EPA and DHA have identical benefits in preventing cardiovascular risk, and since commercial products often have higher EPA concentrations, many simply assume that EPA must be of greater benefit. However, Mori and Woodman concluded back in 2006 that: “The data in humans suggest that DHA may be more favorable in lowering blood pressure and improving vascular function, raising HDL cholesterol and attenuating platelet function. Future studies will need to carefully assess the independent effects of EPA and DHA on other clinical and biochemical measures before decisions can be made with respect to dietary supplements and the fortification of foods with either EPA or DHA.”1
A systematic review, published in 2018 has concluded nearly the same thing: “Both EPA and DHA lowered triglyceride concentration, with DHA having a greater triglyceride-lowering effect. Whilst total cholesterol levels were largely unchanged by EPA and DHA, DHA increased high-density lipoprotein (HDL) cholesterol concentration, particularly HDL₂, and increased low-density lipoprotein (LDL) cholesterol concentration and LDL particle size. Both EPA and DHA inhibited platelet activity, whilst DHA improved vascular function and lowered heart rate and blood pressure to a greater extent than EPA.”2 Below we will explore the data behind these statements, detailing the available evidence which suggest the superiority of DHA for cardiovascular risk prevention.
Triglyceride (TG) Reduction: One of the most consistent lipoprotein marker changes resulting from consumption of EPA and DHA preparations is the reduction in fasting and post-prandial serum TG. Approved omega-3 pharmaceutical products are indicated only for severe hypertriglyceridemia (TG > 500 mg/dl). In general, both EPA and DHA (and combination products) reduce fasting TG by up to 50%, which is both dose-dependent and influenced by baseline TG levels (higher baseline TG results in greater potential reduction). 3 When compared head-to-head, DHA appears to have a greater ability to lower TG levels, though the differences between DHA and EPA are often not statistically different.4
LDL, HDL and non-HDL cholesterol: There is much controversy surrounding the ability of fish oil supplement to affect LDL-C and HDL-C levels; especially related to their ability to raise LDL-C. Research shows that DHA supplementation raises both HDL-C and LDL-C, though it does not increase non-HDL-C. These changes in both HDL-C and LDL-C appear to be greater where TG-lowering is greatest. [Allaire],5 Since the increase in LDL-C does not translate to higher non-HDL-C, this is likely the result of shifting cholesterol from VLDL particles to LDL and HDL particles, which then shifts LDL particles toward a larger and less atherogenic phenotype (see discussion below on particle size changes). The increase in LDL-C (and HDL-C) after DHA supplementation should therefore be viewed as metabolically favorable and indicative of a shifting of lipids away from the triglyceride-rich VLDL particles.
Lipoprotein Particle Size: Combinations of EPA and DHA have been shown to favorably alter lipoprotein particle size: increasing both LDL and HDL particle sizes as well as decreasing VLDL particle size. When EPA and DHA are compared with respect to their ability to improve HDL particle size, DHA-rich oils show more consistent improvements.6 This may be due to the fact that DHA has a greater inhibition of cholesterol ester transfer protein (CETP) activity, one of the enzymes responsible for altering lipoprotein particle size.7 DHA, but not EPA was capable of increasing LDL particle size in treated hypertensive type 2 diabetic patients as well as overweight hypercholesterolemic subjects.5 ,8
Hypertension: Omega-3 fatty acids have shown modest improvements in both blood pressure measurements and endothelial function, particularly in hypertensive patients.9, 10,11 In animal and human studies, DHA supplementation had a more significant impact on reducing both systolic and diastolic blood pressure than did EPA supplementation.12 DHA also showed more improvement on endothelial function in these patients.13 Both EPA and DHA improve arterial compliance. 5,14
Heart Rate: An increased heart rate is an independent risk factor for CVD mortality. In a study comparing DHA to EPA in their ability to affect heart rate; DHA was able to lower heart rate in overweight hyperlipidemic men while EPA was not.5 Other studies have shown similar superiority of heart rate lowering using DHA as compared to EPA. 15, 16
Conclusion and Recommendation: While many advocates of omega-3 fatty acid therapy have suggested that products containing a 3:2 or 2:1 ratio of EPA:DHA are the most appropriate for CVD prevention and treatment, the data in humans suggests otherwise. In nearly every surrogate marker in which EPA or DHA results differ, there is evidence to suggest that DHA is superior to EPA. While no large clinical trial has been performed that distinguishes these differences in hard end-points (MI, CVD mortality), among post-menopausal women with atherosclerosis (detected by coronary angiography) followed for over 3 years, serum DHA levels above the median were statistically correlated with reduced atherosclerotic progression and fewer lesions.17 Neither EPA nor ALA levels showed any correlation with changes in atherosclerotic progression. This corresponds to other epidemiological data showing DHA levels to be more closely tied to reducing risk compared to other fatty acids, including EPA.18, 19 Research has also recently shown that when consuming equal doses of EPA or DHA, the omega-3 index increases to a greater extent in those consuming DHA.20
Therefore, for both primary prevention in patients with increased CVD risk and secondary CVD prevention, we believe there is enough evidence to suggest that clinicians who use omega-3 fatty acid therapy should recommend products with a higher content of DHA than EPA (though not necessarily DHA-alone). When omega-3 fatty acid therapy is being recommended for general health in patients with low risk for CVD, choosing an EPA:DHA ratio which reflects other desired outcomes (e.g., depression, eye health etc.) is likely to reduce cardiovascular risk as well.

Thomas G. Guilliams, PhD (Tom) earned his doctorate in molecular immunology from the Medical College of Wisconsin in Milwaukee. For the past two decades, he has spent his time investigating the mechanisms and actions of lifestyle and nutrient-based therapies, and is an expert in the therapeutic uses of dietary supplements. Tom serves as an adjunct assistant professor at the University of Wisconsin School of Pharmacy and was the VP of Science for Ortho Molecular Products for 24 years (he now serves them as a consultant). Since 2014 he has been writing a series of teaching manuals (Road Maps) that outline and evaluate the evidence for the principles and protocols that are fundamental to the functional and integrative medical community. He is the founder and director of the Point Institute, an independent research and publishing organization that facilitates the distribution of his many publications. A frequent guest-speaker, Dr. Guilliams provides training to a variety of health care disciplines in the use of lifestyle and natural medicines. He lives in the woods outside of Stevens Point, Wisconsin with his wife and children.
References
1 Mori, T.A. and Woodman, R.J. The independent effects of eicosapentaenoic acid and docosahexaenoic acid on cardiovascular risk factors in humans. Curr Opin Clin Nutr Metab Care. 2006; 9(2):95-104.
2 Innes JK, Calder PC. The Differential Effects of Eicosapentaenoic Acid and Docosahexaenoic Acid on Cardiometabolic Risk Factors: A Systematic Review. Int J Mol Sci. 2018 Feb 9;19(2).
3 Backes J, Anzalone D, Hilleman D, Catini J. The clinical relevance of omega-3 fatty acids in the management of hypertriglyceridemia. Lipids Health Dis. 2016 Jul 22;15(1):118.
4 Allaire J, Couture P, Leclerc M, et al. A randomized, crossover, head-to-head comparison of eicosapentaenoic acid and docosahexaenoic acid supplementation to reduce inflammation markers in men and women: the Comparing EPA to DHA (ComparED) Study. Am J Clin Nutr. 2016 Aug;104(2):280-7.
5 Mori TA, Burke V, Puddey IB, et al. Purified eicosapentaenoic and docosahexaenoic acids have differential effects on serum lipids and lipoproteins, LDL particle size, glucose, and insulin in mildly hyperlipidemic men. Am J Clin Nutr. 2000 May;71(5):1085-94.
6 Buckley, R.; Shewring, B. et al. Circulating triacylglycerol and apoE levels in response to EPA and docosahexaenoic acid supplementation in adult human subjects. Br J Nutr. 2004; 92(3):477-483.
7 Hirano, R.; Igarashi, O. et al. Regulation by long-chain fatty acids of the expression of cholesteryl ester transfer protein in HepG2 cells. Lipids. 2001; 36(4):401-406.
8 Woodman, R.J.; Mori, T.A. et al. Docosahexaenoic acid but not eicosapentaenoic acid increases LDL particle size in treated hypertensive type 2 diabetic patients. Diabetes Care. 2003; 26(1):253
9 Zehr KR, Walker MK. Omega-3 polyunsaturated fatty acids improve endothelial function in humans at risk for atherosclerosis: A review. Prostaglandins Other Lipid Mediat. 2018 Jan;134:131-140.
10 Balakumar P, Taneja G. Fish oil and vascular endothelial protection: bench to bedside. Free Radic Biol Med. 2012 Jul 15;53(2):271-9.
11 Cicero AF, Ertek S, Borghi C. Omega-3 polyunsaturated fatty acids: their potential role in blood pressure prevention and management. Curr Vasc Pharmacol. 2009 Jul;7(3):330-7.
12 Mori, T.A.; Bao, D.Q. et al. Docosahexaenoic acid but not eicosapentaenoic acid lowers ambulatory blood pressure and heart rate in humans. Hypertension. 1999; 34(2):253-260.
13 Mori, T.A.; Watts, G.F. et al. Differential effects of eicosapentaenoic acid and docosahexaenoic acid on vascular reactivity of the forearm microcirculation in hyperlipidemic, overweight men. Circulation. 2000; 102(11):1264-1269.
14 Nestel P, Shige H, Pomeroy S, et al. The n-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid increase systemic arterial compliance in humans. Am J Clin Nutr. 2002 Aug;76(2):326-30.
15 Grimsgaard, S.; Bonaa, K.H. et al. Effects of highly purified eicosapentaenoic acid and docosahexaenoic acid on hemodynamics in humans. Am J Clin Nutr. 1998; 68(1):52-59.
16 Hidayat K, Yang J, Zhang Z, et al. Effect of omega-3 long-chain polyunsaturated fatty acid supplementation on heart rate: a meta-analysis of randomized controlled trials. Eur J Clin Nutr. 2017 Dec 28. doi: 10.1038/s41430-017-0052-3.
17 Erkkila, A.T.; Matthan, N.R. et al. Higher plasma docosahexaenoic acid is associated with reduced progression of coronary atherosclerosis in women with CAD. J Lipid Res. 2006; 47(12):2814-2819.
18 Albert, C.M.; Campos, H. et al. Blood levels of long-chain n-3 fatty acids and the risk of sudden death. N Engl J Med. 2002; 346(15):1113-1118.
19 Simon, J.A.; Hodgkins, M.L. et al. Serum fatty acids and the risk of coronary heart disease. Am J Epidemiol. 1995; 142(5):469-476.
20 Allaire J, Harris WS, Vors C, et al. Supplementation with high-dose docosahexaenoic acid increases the Omega-3 Index more than high-dose eicosapentaenoic acid. Prostaglandins Leukot Essent Fatty Acids. 2017 May;120:8-14.