Adapted from the MSK Solutions In-Practice Guide, Lifestyle Matrix Resource Center, 2018.
Patient Presentation
A 49-year-old female presents with persistent widespread pain and fatigue for the last five months. Her body map chart shows that the painful areas cover muscles below the waist following the paraspinals, scapula, trapezius and occiput. She also complains of frequent migraine headaches and numbness and tingling in right and left hands. She gets numbness in her right foot but denies LBP or radiating pain. She shared that she has fatigue, stiffness, unrefreshing sleep, cognitive difficulties, anxiety, occasional depression and functional impairment of activities of daily living (ADLs).
She says she has a child with cerebral palsy that lives at home and requires constant care. Symptoms are without definitive organic origin. She is on Lyrica® for the fibromyalgia from her primary care doctor but gets mixed results. She is also on metformin to help manage her blood sugar fluctuations and has been told she is prediabetic. She has tried acupuncture, chiropractic, physical therapy and different doctors, but she has not found lasting relief.
During the exam, she also mentions she has TMJ. She rates her pain as a 6/10 on average, but reaches a 7-8/10 when she tries to exercise (walking). Extremely tender on physical exam and “everything” hurts when she is touched. She demonstrates normal ROM, strength, reflexes, cranial nerves and vision but elevated BP and HR. She wants to try an alternative to Lyrica® because it makes her dizzy when she stands up and gives her blurry vision. Past lab tests indicate there is currently no organic disease.
Fibromyalgia Background Information for Practitioners
Central Nervous System Sensitization
The fibromyalgia syndrome (FMS) research and medical literature has recently focused around the concept of central sensitization—often called central allodynia or classic fibromyalgia. The CNS undergoes a neural adaptation where it processes sensory stimuli abnormally, resulting in an amplified perception of stimuli (hyperalgesia), such as light touch being perceived as pain. This plasticity of the CNS is thought to result from significant acute or chronic stress, including chronic pain, physical or psychological trauma, or other stressors, which can result in limbic system dysfunction and failure of the descending antinociceptive system (DANS).
Studies of a variety of thermal, mechanical and electrical stimuli in FMS and healthy controls consistently show increase in reactivity in the FMS group, suggestive of central sensitization. PET scans and fMRI studies of the brain activity of FMS subjects versus healthy controls while they receive innocuous sensory stimulation have shown that FMS patients’ limbic structures and CNS pain areas are activated by nonpainful stimuli that only activate the sensory cortex in healthy controls.
Hypervigilance
Recent medical literature has observed a decrease in serotonin, an increase in substance P, a pain modulating peptide, in the CNS, and disordered catecholamine production in patients with FMS. Other alterations in neurotransmitter levels have been reported, such as decreases in dopamine, oxytocin and acetylcholine levels, along with increased NMDA (N-methyl-D-aspartate) activity. Collectively, these changes have been found to be associated with a generalized state of hypervigilance (sympathetic overactivity), resulting in associated autonomic phenomenon, such as irritable bowel/bladder syndrome, anxiety, depression, and disordered nonrestorative sleep, which are also commonly seen in hypervigilant patients with post-traumatic stress disorder (PTSD).
Hypothalamic Dysfunction
Hypothalamic dysfunction is also generally present in FMS. The hypothalamus is a major control center for sleep, and impaired function contributes to nonrestorative sleep. As a regulator of autonomic function, hypothalamic dysfunction contributes to the many symptoms of dysautonomia or somatic symptoms, including sweating and irritable bowel syndrome. The hypothalamus is also involved in hormonal regulation.
Hormonal Dysfunction
Hormonal dysfunction, including hypothyroidism, is often present, as is poor sleep, which further decreases energy production, preventing resolution of the FMS. Studies have shown differences in circadian cortisol release in FMS versus healthy controls, suggestive of initial overactivity followed by later exhaustion of the hypothalamic-pituitary-adrenal (HPA) axis. This can include blunting of cortisol release in the morning, along with levels being too high in the evening, which may then disrupt sleep.
Treatment Strategy
Two studies, including an RCT by Teitelbaum et al., showed an average 90% improvement rate in FMS,
along with a marked decrease in pain, when using the S.H.I.N.E.® protocol: sleep treatment, hormonal support, infections, nutritional support and exercise (to patient tolerance).
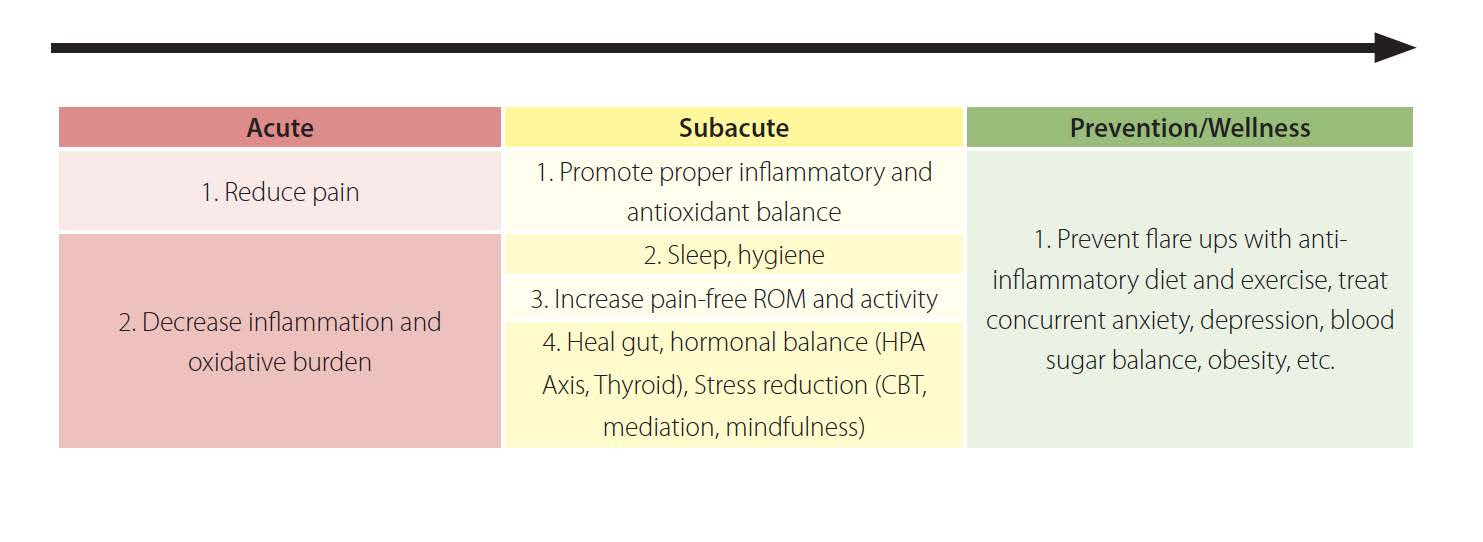
Goals (six months to one year):
Treatment Protocol
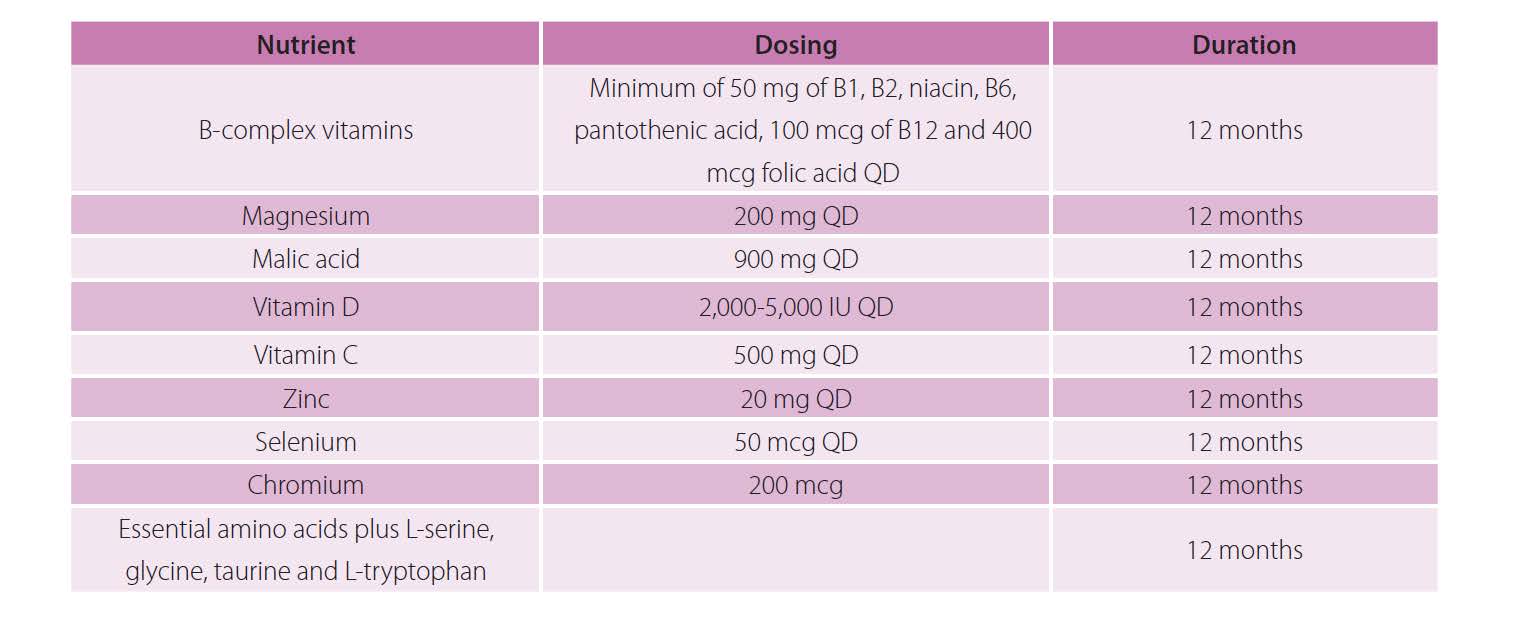
High-quality multivitamin with combined nutrients taken long-term (multiple years) that contains the following:
Added optional nutrient support, including mitochondrial support (energy), ATP production support, and inflammatory and antioxidant support: 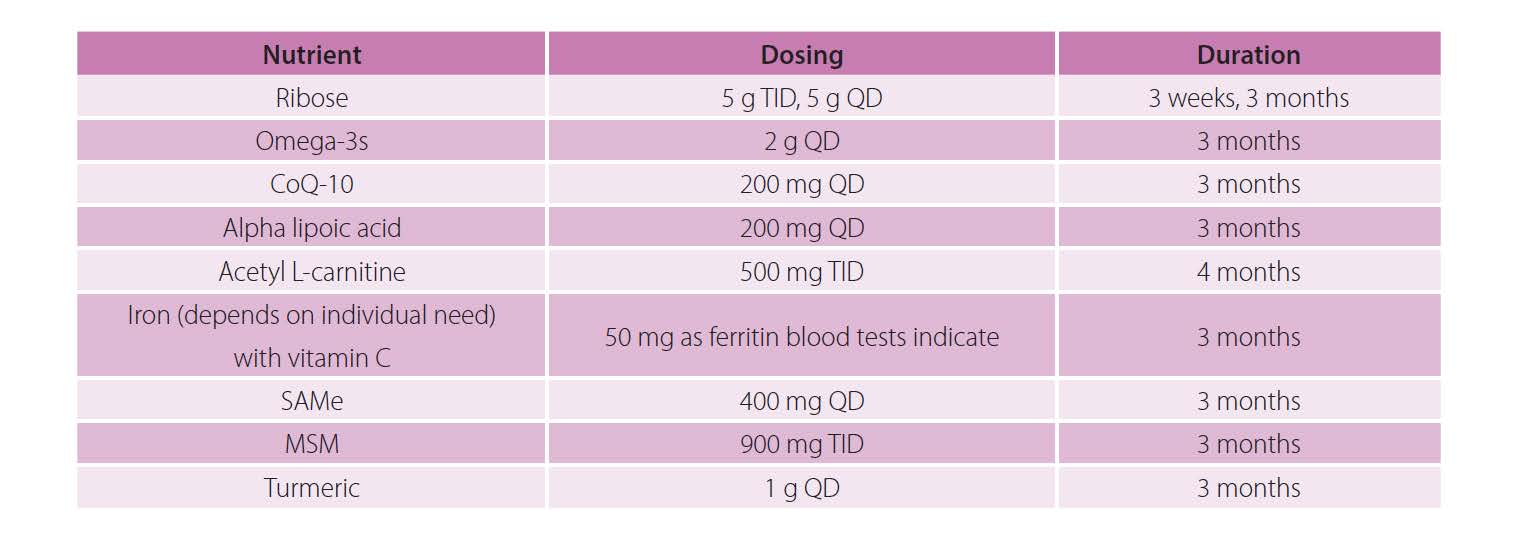
Sleep support: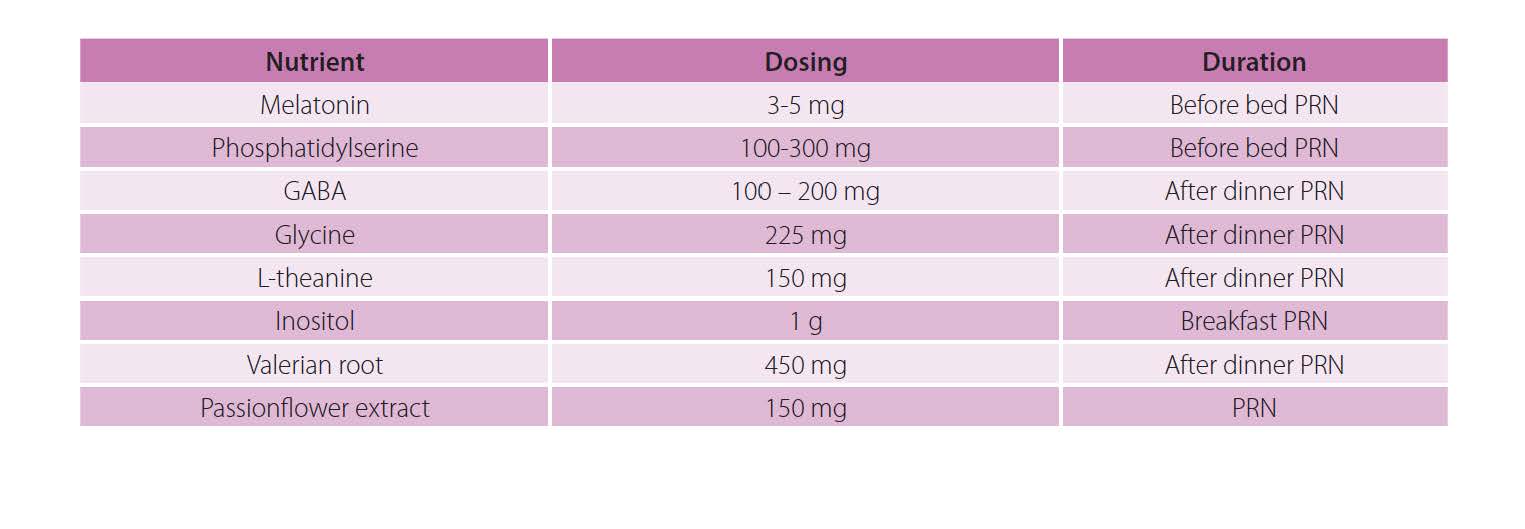
Fibromyalgia Rehabilitation
A successful fibromyalgia rehabilitation program involves not only a multidisciplinary team of professionals (e.g., physician, mental health professional, chiropractor, physical and massage therapists, exercise professional) with expertise in the treatment of soft-tissue disorders but also includes various modalities (e.g., exercise, education, mindfulness, meditation, cognitive behavioral therapy, finding and avoiding pain triggers through journaling) individualized for each patient.
Traditional therapy or rehabilitation may worsen the patient’s symptoms. Monitor the progress of the patient during rehabilitation. As goals are met and symptoms change, modify the rehabilitation prescription to meet the individual’s current needs.

Educated in both the Netherlands and the United States, Adrian den Boer, ND, DC, IFMCP is a board-certified and licensed naturopathic and chiropractic physician. In addition, Dr. den Boer is fully certified as a functional medicine doctor. Dr. den Boer has treated over 10,000 patients successfully by utilizing multiple resources to manage patient care. Most recently, he joined the Lifestyle Matrix Resource Center as the Clinical Expert serving the MSK Solutions Pain Recovery Program.