Let’s face the facts: If you see human patients, you're seeing patients with metabolic dysfunction.
Even children, who should be resilient and thriving, are showing signs of metabolic dysfunction.
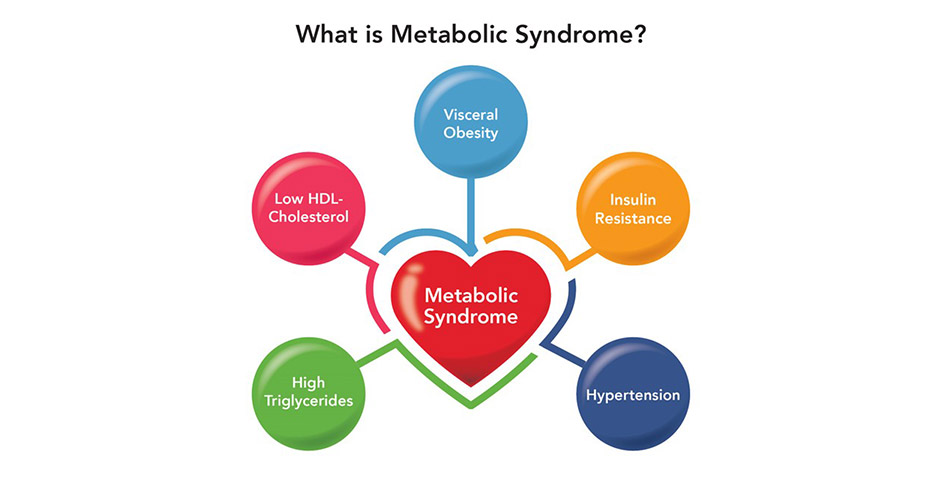
Think back to the average patient walking through your doors (or on your virtual appointment calendar). It's rare to not see at least one or two aspects of metabolic syndrome.
With most adults in the United States estimated to be on at least four different prescription medications, patients expect this approach and have been conditioned to want a pill for an ill. But of course, we know there is a better way with functional medicine. It’s one of the reasons some patients seek out the care of a functional medicine practitioner.
Perhaps you have even had conversations start with, "You're the doc that doesn’t like drugs, right?"
But with guidelines outlining the standard of care, is remission from metabolic disease even possible? Using the example of type 2 diabetes, a growing body of evidence suggests that remission is indeed possible. In fact, in 2009 the American Diabetic Association attempted to categorize remission into three possible scenarios:
- Remission: achieving glycemia below the diabetic range in the absence of active pharmacologic (anti-hyperglycemic medications, immunosuppressive medications) or surgical (ongoing procedures such as repeated replacements of endoluminal devices) therapy
- Partial remission: sub-diabetic hyperglycemia (A1C not diagnostic of diabetes [<6.5%], fasting glucose 100–125 mg/dl [5.6–6.9 mmol/l]) of at least one year’s duration in the absence of active pharmacologic therapy or ongoing procedures
- Complete remission: a return to “normal” measures of glucose metabolism (A1C in the normal range, fasting glucose <100 mg/dl [5.6 mmol/l]) of at least one year’s duration in the absence of active pharmacologic therapy or ongoing procedures.
This is further reinforced in a 2020 review article published by the American College of Lifestyle Medicine, which concluded that there is ample evidence to support the use of lifestyle modification for type 2 diabetes remission and should be the primary treatment and standard of care.
Easier said than done, right?
That’s why we’re here to help by outlining the four critical principles to help your patients reach and maintain remission for all aspects of metabolic syndrome, and avoid a lifetime of pharmaceutical drugs.
Avoid the Immediate Risk
A core principle of functional medicine is that no patient is the same. One patient may not need certain drugs in their initial treatment while another could be the exact opposite! Further, depending on what the patient presents with, drug prescriptions may be necessary to avoid the immediate risk of a heart attack or stroke, allowing you time to initiate the necessary lifestyle interventions.
Said another way, pharmaceuticals like statins, metformin and common blood pressure medications are not evil; they are simply tools. The issues arise when patients are not regarded as a partner in their treatment, but simply subordinates who should do what they are told and take the drugs prescribed.
In contrast, we encourage collaboration with patients in their health journeys. This allows the provider to set expectations on the front-end, use pharmaceuticals only if needed, and initiate a lifestyle intervention that both the patient and provider can get behind.
Build Metabolic Reserve
If we were only dealing with sedentary adolescents and teens, this would more straightforward, as teens presenting with obesity and diabetic risk can reach remission much faster than their senior counterparts who have been chipping away at their metabolic reserves and resilience for a decade or more.
For our higher-risk patients, we will need to consider secondary supplemental support.
Supplements should be considered for many patients, because like prescription drugs, they help avoid the immediate risk. Most importantly, unlike prescription drugs, well-researched supplements do not deplete key vitamins and minerals or come with unwanted side effects. Unfortunately, all supplements are not created equal. A quick search on Amazon for “heart health supplements” gives a deluge of matches (over 6,000 results!), most offering little value.
There are, however, a few nutrients that rise to the top when we think of cardiovascular and metabolic risk. The following should be included in any supplement protocol for the metabolic syndrome patient:
- Fish oil: There are few supplements that have been researched more than omega-3 fatty acids. The strongest research shows that a blend of EPA, DHA, and DPA can improve cardiovascular health, lower inflammation and support cognitive development and function. While a select few studies call the benefit of supplementing omega-3 fatty acids into question, a recent systematic review of over 100,000 subjects concluded that no further research is needed; there is simply enough evidence to state that omega-3 supplementation lowers the risk of cardiovascular disease.
- Berberine: Often described as nature’s metformin, berberine has been used for thousands of years for a variety of conditions. Modern research has shown berberine can improve diabetic markers, including hbA1c and fasting blood glucose, in a manner comparable to metformin and can improve lipid measurements such as TC, LDL-C and triglyceride measurements superior to metformin.
- Bergamot: Commonly seen as a flavoring in Earl Gray tea, this citrus fruit has been consumed as a heart-healthy drink in the costal Calabrian region of Italy for centuries. The locals’ resilience against heart disease prompted research that found many rare polyphenol flavonoids in the bergamot fruit that possess diverse mechanisms to modulate cholesterol production in the liver, lower cholesterol absorption in the GI tract, and provide anti-inflammatory and antioxidant activity without impacting CoQ-10 levels.
Implement Community Care
If you have been following LMRC for a while, you know we're fans of group visits. With group visits having many benefits, from increased patient satisfaction and outcomes, higher patient knowledge and community support, there are few care models better suited for the metabolic syndrome patient.
The great news is with a relaxation of previous regulations surrounding HIPAA and telemedicine, group visits conducted on Zoom post-2020 are here to stay.
Attract the Right Patients
However, even when you do everything right, if the patient is not ready, willing, or able to make lifestyle changes, you will lose valuable time and energy in exchange for stress and frustration.
Getting the right patients walking through your doors (or onto your virtual appointment calendar) is just as important!
Successful practitioners have several systems that help them stand out from the pack:
- A specific patient avatar they aim to attract to their practice
- Lead magnets on social media and/or their website designed to speak to their ideal patient and collect contact information
- A successful nurture process designed to lead the patient from contemplation to making their first appointment
- A well-structured patient journey utilizing patient education resources and group visits to create engagement, understanding and lasting behavior change
- A follow-up plan design to transition patients from treatment to maintenance
Need a Hand?
At LMRC, we have taken the guesswork out of functional medicine implementation with our NEW Onboarding Portal, a five-module mini-course that:
- Helps you effectively implement a niched functional medicine program into your practice
- Gives you the tools and strategy to market the program to current and prospective clients
- Expands your clinical knowledge so you can become the go-to expert in your community
Set up a free concierge call to discuss your unique practice needs with one of our implementation specialists.

Steven Imgrund is a board-certified nutritionist. Steven developed his passion for nutrition and health working as personal trainer and health coach, specializing in weight loss and behavior change. Through working with hundreds of clients, Steven has seen the challenges with implementing long-term lifestyle and dietary habits. This experience has fueled his passion for functional medicine, and his desire to help health care practitioners use proven lifestyle and supplement strategies to safely address the root causes of their patients cardiometabolic issues. Steven received his Masters in Human Nutrition through Bridgeport University in 2018, and Certified Nutrition Specialist (CNS) certification in 2020.



